Biologics: Transforming Autoimmune Disease Care
Autoimmune diseases such as psoriasis and rheumatoid arthritis affect millions worldwide. Biologics and their more affordable counterparts, biosimilars, have reshaped treatment strategies by precisely targeting immune system pathways to reduce symptoms and improve overall quality of life.
Autoimmune diseases such as psoriasis and rheumatoid arthritis affect millions worldwide. Biologics and their more affordable counterparts, biosimilars, have reshaped treatment strategies by precisely targeting immune system pathways to reduce symptoms and improve overall quality of life.
Understanding Autoimmune Diseases and Their Effect on Skin Health
Autoimmune disorders arise when the body’s immune defenses mistakenly attack its own cells, tissues, or organs. These conditions can impact multiple body systems, including the skin, resulting in visible dermatological symptoms.
1. Common Autoimmune Skin Disorders
Several autoimmune conditions primarily manifest on the skin. Psoriasis causes thick, scaly plaques. Lupus may present with a butterfly-shaped facial rash. Scleroderma results in hardened, thickened skin, while dermatomyositis produces muscle weakness alongside distinctive rashes.
2. Biologics in Modern Treatment
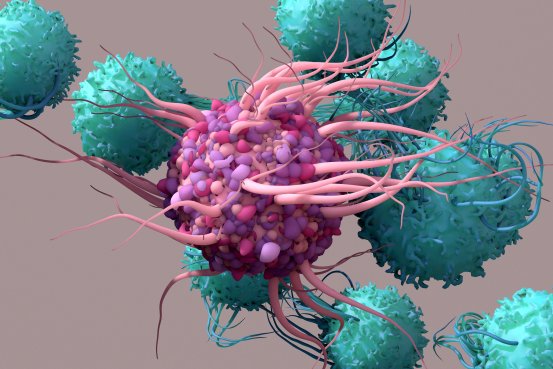
Biologics are drugs developed from living cells that specifically target immune system components involved in inflammation. They are often prescribed when conventional therapies fail to control disease activity.
3. Types of Biologics for Skin Conditions
Widely used biologics include TNF-alpha inhibitors (etanercept, adalimumab, infliximab), IL-17 inhibitors (secukinumab, ixekizumab), and IL-23 inhibitors (guselkumab, tildrakizumab). These agents are most often prescribed for psoriasis, psoriatic arthritis, and similar immune-related skin diseases.
4. How Biologics Function
By blocking specific immune signals, biologics help reduce inflammation. TNF-alpha inhibitors neutralize tumor necrosis factor-alpha, a major inflammatory protein, while IL-17 and IL-23 inhibitors interfere with interleukins that contribute to skin inflammation.
5. Advantages of Biologic Therapy
Patients frequently see marked improvement in symptoms, including clearer skin, reduced inflammation, and less pain, leading to better quality of life.
6. Potential Risks and Side Effects
Because biologics suppress immune function, infection risk is higher. Side effects may include mild respiratory infections, localized injection reactions, and allergic responses. Though uncommon, serious infections or certain cancers can occur.
7. Ongoing Monitoring
Biologic use requires regular checkups to detect infections or other adverse effects early. Blood work is typically performed at intervals to ensure patient safety.
| Biologic Class | Examples | Common Uses |
| TNF-alpha Inhibitors | Etanercept, Adalimumab, Infliximab | Psoriasis, Psoriatic Arthritis |
| IL-17 Inhibitors | Secukinumab, Ixekizumab | Psoriasis |
| IL-23 Inhibitors | Guselkumab, Tildrakizumab | Psoriasis |
Source: National Psoriasis Foundation, 2024
Biologics in the Broader Management of Autoimmune Diseases
Biologics have set a new standard in autoimmune care by offering targeted treatments that significantly reduce disease activity and improve daily living.
1. Defining Biologics
Derived from living sources such as cells or bacteria, biologics include monoclonal antibodies, recombinant proteins, and fusion proteins. Unlike synthetic drugs, these therapies are large, complex molecules designed to focus on specific immune targets.
2. Mechanisms of Action
Biologics selectively block immune pathways that drive inflammation. Some neutralize TNF-α, others inhibit IL-6, and some reduce B-cell activity to limit harmful antibody production. By disrupting these pathways, biologics help preserve healthy tissue.
3. Conditions Commonly Treated
These therapies are used for rheumatoid arthritis, Crohn’s disease, ulcerative colitis, psoriasis, and multiple sclerosis, helping reduce symptoms, control disease progression, and prevent long-term complications.
4. Main Biologic Categories
Options include TNF-α inhibitors (adalimumab, infliximab), IL-6 inhibitors (tocilizumab), B-cell depleting drugs (rituximab), and T-cell modulators (abatacept). The choice depends on the patient’s diagnosis, disease severity, and health profile.
5. Clinical Benefits
Trials show biologics can ease symptoms, prevent joint destruction, and restore physical function when other treatments fall short.
6. Risks to Consider
Side effects range from mild injection site reactions to higher vulnerability to opportunistic infections. Rare but serious events include allergic responses and certain cancers.
Home Remedies for Itchy, Dry Scalp
A dry, itchy scalp can be treated with accessible home-based approaches.
1. Natural Oils
Coconut, olive, and jojoba oils restore moisture and relieve itching. Apply warm oil, massage, and leave for 30 minutes or overnight before rinsing.
2. Apple Cider Vinegar Rinse
Balances scalp pH and reduces yeast growth; dilute 1:1 with water, apply post-shampoo, leave briefly, and rinse.
3. Aloe Vera
Soothes irritation and reduces inflammation; apply gel for 15–20 minutes before rinsing.
4. Oatmeal Paste
Finely ground oatmeal mixed with water calms irritation; apply for 10–15 minutes.
5. Tea Tree Oil
Antifungal and antibacterial; mix with a carrier oil, massage in, and rinse after 30 minutes. Always patch test first.
Biosimilars: Expanding Access to Autoimmune Treatments
While biologics can be costly, biosimilars make therapy more affordable without compromising safety or effectiveness.
1. What Are Biosimilars?
They closely resemble approved biologics in quality, safety, and efficacy, but are not identical generics. They must undergo rigorous comparison studies.
2. Use in Autoimmune Care
Many biosimilars target TNF-alpha to treat rheumatoid arthritis, Crohn’s disease, and psoriasis, performing comparably to their reference biologics.
3. Cost and Availability
Biosimilars reduce treatment costs, improving access for patients who previously could not afford biologics.
4. Safety Considerations
Concerns about immune reactions are generally unfounded, as research shows switching between a biologic and its biosimilar is typically safe under medical guidance.
Emerging Innovations in Autoimmune Disease Management
1. Advanced Targeted Therapies
New biologics and immunomodulators are even more precise, limiting side effects while improving disease control—e.g., IL-17 inhibitors for psoriasis.
2. Cell-Based Treatments
Techniques like CAR-T cell therapy and stem cell transplants are being tested for severe autoimmune disorders, with early signs of possible long-term remission.
3. Nanotechnology in Drug Delivery
Nanoparticles enable targeted delivery, reducing systemic exposure and improving drug effectiveness with fewer side effects.
Q&A
Q1: What are autoimmune diseases, and how do they affect the skin?
A1: They occur when the immune system attacks the body’s own tissues, producing skin conditions like psoriasis, lupus, scleroderma, and dermatomyositis.
Q2: How do biologics work in autoimmune skin disorders?
A2: By blocking immune proteins such as TNF-alpha or interleukins, they reduce inflammation and ease symptoms.
Q3: What biologic types are used for these conditions, and what are their pros and cons?
A3: TNF-alpha inhibitors, IL-17 inhibitors, and IL-23 inhibitors can clear skin and reduce pain but increase infection risk and may cause rare severe side effects.
Q4: How do biologics differ from biosimilars?
A4: Biologics are original therapies, while biosimilars are highly similar, equally effective, and usually more affordable.
References
https://www.numberanalytics.com/blog/ultimate-guide-biologics-autoimmune-skin-diseases
https://www.uspharmacist.com/article/the-expanding-role-of-biosimilars-in-autoimmune-diseases
https://www.autoimmuneinstitute.org
https://www.numberanalytics.com/blog/biologics-for-autoimmune-skin-diseases
https://ameripharmaspecialty.com/ivig/ivig-and-autoimmune-diseases/
